Introduction
During the 2003–2005 period, 442 patients with burn injuries (an average of 147 per year) were admitted to the Department of Burn Injuries, University Hospital of Traumatology in Zagreb. The most common causes of burn injury were flame (fire, 41%) and hot liquids (scalds, 31%), followed by contact burns, electrical burns, explosions and chemical burns.
Burns are extremely complex traumatic injuries that can be classified according to burn depth, size and area involved in injury, age and general health status (1-3). In treatment planning, it is essential to estimate the extent of burn wound which is expressed by means of percentage of total body surface area (%TBSA). The so-called rule of nines is most commonly applied in adults to estimate the extent of burn wound: the body is divided into areas and each area is attributed a multiple of the number nine. The head with the neck and the upper limbs account for 9% each, anterior and posterior trunk 18% each, each lower limb 18% of body surface, the remaining 1% accounts for the genitalia and perineum. Thermal trauma leads to impairment of skin structure and loss of skin functions. Tissue damage is the direct result of heat coagulation of structural proteins, while further progression of injury depends on the release of local mediators, changes in microcirculation, tissue edema and infection (1, 2). Burned patients are characterized by severe impairment of hemostatic balance and immune response, and platelets play an important role in the modulation of both these responses.
Platelets are small fragments of megakaryocyte cytoplasm. They play a fundamental role in primary and secondary hemostasis, as crucial reactions of the coagulation cascade occur on their phospholipid surface. The early phase of acute burn is characterized by a bleeding tendency, whereas the late phase is characterized by hypercoagulability (4). Although the platelet primary function is hemostatic regulation, they also act as inflammatory cells. They release inflammatory mediators, express proinflammatory surface molecules, interact with leukocytes and endothelial cells, thus taking part in the induction of acute and chronic immune response (5-7). If TBSA exceeds 30%, the released inflammatory mediators and cytokines migrate to the systemic circulation, inducing systemic inflammatory response to injury. Infections are the leading cause of death in patients who survive the initial period of treatment; they are the consequences of impairments in cellular and humoral immune responses in patients with severe burns (1, 2).
Studies investigating the role of platelets and platelet count in burn patients are rare, rather old and mostly presenting case reports. The Department of Burn Injury of our University Hospital is one of the leading centers in Croatia specialized in this type of injury, thus it is understandable that investigations of pathophysiologic disorders in burn patients are of great interest, not only in understanding the clinical course of burn wound, but also in monitoring the efficacy of treatment applied and early prognosis of complications and disease outcome. The aim of the present study was to monitor platelet count in groups of patients with different percentage of body surface area burned (≤ 10% TBSA – group A; > 10% TBSA – group B), and with regard to the outcome of disease (survival/death).
Materials and methods
Patients
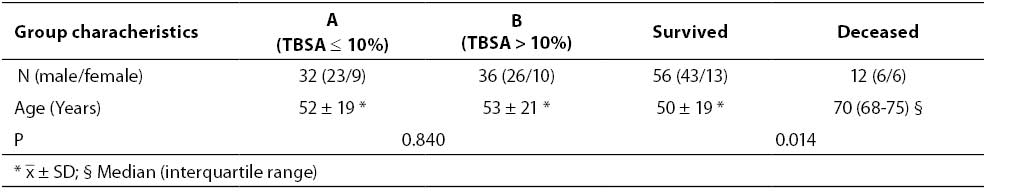
Retrospectively, of a total of 442 burn patients who were treated in a 3-year period, we selected and included in the study 68 patients with appropriate blood sampling dynamics on days 1, 4, 7, 14, 21, 28 after burn injury, and depending on the length of hospital stay at the Department of Burn Injury, University Hospital of Traumatology Zagreb. Patients referred to our University Hospital from other institutions for additional care and treatment (those that were not admitted immediately after being injured), and patients with inappropriate blood sampling dynamics were excluded. A total of 49 male and 19 female patients, mean age 55 (35-70) years (median, interquartile range), were investigated. Burn patients were divided in groups A and B, depending on the percentage of total body surface area burned. Group A consisted of 32 patients with mild burns (≤ 10% TBSA), whereas group B consisted of 36 patients with moderate/severe burns (> 10% TBSA). Group B consisted of 20 patients with TBSA 11–20%, 9 patients with TBSA 21–40%, 6 patients with TBSA 41–60% and 1 patient with TBSA > 61%. Depending on disease outcome, patients were subsequently divided into two groups: 56 patients who survived, and 12 patients who died as a consequence of burn injury. Basic burn patient group characteristics are shown in Table 1. This study was approved by the Ethics board of the University Clinic of Traumatology, Zagreb.
Methods
Platelet count was determined as a part of routine patient work-up and follow up, in whole blood samples with the addition of K3EDTA as anticoagulant, using the automated hematology analyzer Sysmex-XT 1800i (Sysmex Corporation, Kobe, Japan).
Statistical analysis
Variables were tested for normality using the Kolmogorov-Smirnov test. Parametric data were expressed as arithmetic mean and standard deviation, with the pertaining 95% confidence interval, whereas nonparametric data were expressed as median and interquartile range, with the pertaining 95% confidence interval. The t-test and Mann-Whitney test were used for between-group difference testing of parametric and nonparametric data, respectively. Differences in platelet count between multiple time points within groups were tested using the RM ANOVA. Differences in platelet count between paired time points within groups were tested using a post hoc test (Holem Sidak). Values of P < 0.05 were considered statistically significant. Analyses were performed using the Sigmastat for Windows software, version 3.5, Systat Software Inc.
Results
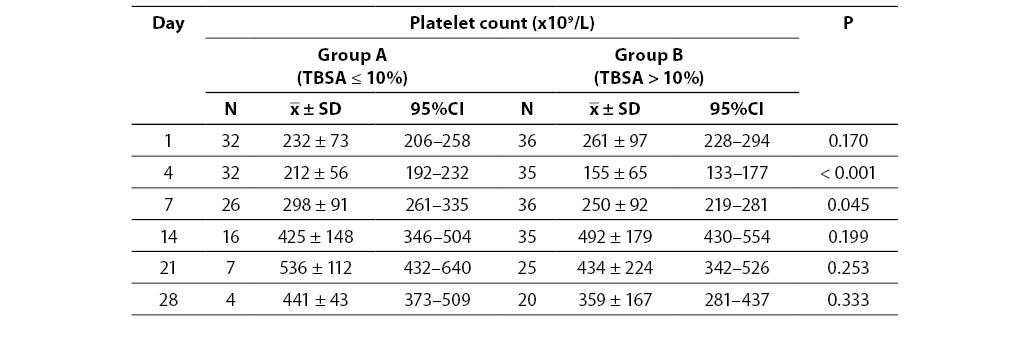
No significant difference was observed in patient age (P = 0.840) comparing group A and B according to severity of burn injury, but the difference in patient age was found comparing groups according to disease outcome. Patients with lethal outcome were significantly older compared to surviving patients (P = 0.014) (Table 1). Only one patient from group A died; he was 70 years old. The remaining 11 patients who died were from group B (3 with TBSA 11-20%, 2 with TBSA 21-40%, 5 with TBSA 41-60% and 1 with TBSA > 61%).
Table 1. Characteristics of burn patient groups
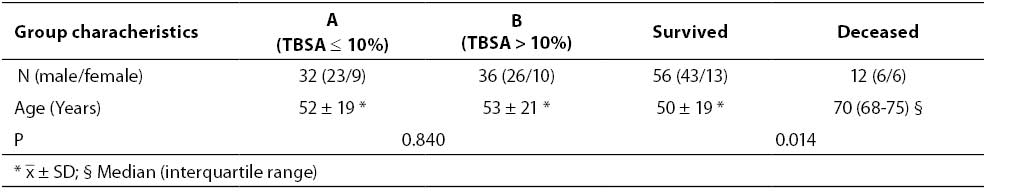
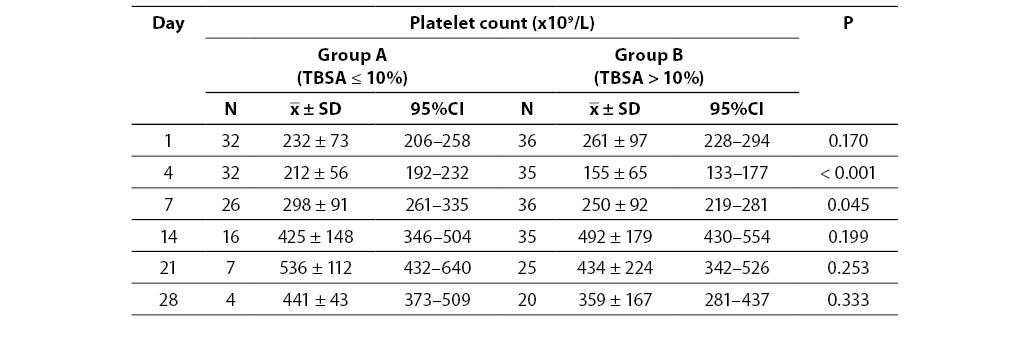
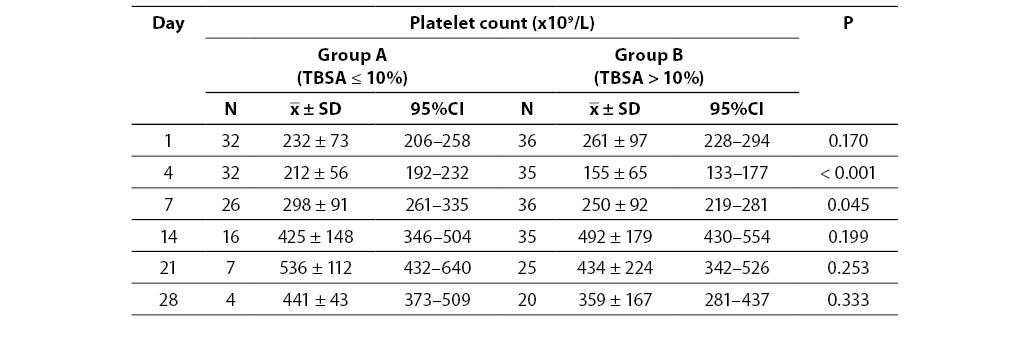
Platelet count in investigated burn patient groups according to severity of injury is shown in Table 2. On the first day of investigation, platelet count was within the reference range (158-424 x 109/L), showing no significant difference between groups (P = 0.170). On the contrary, on the 4th and 7th day of platelet count monitoring, there was a significant between-group difference, platelet count was lower in group B (P < 0.001; P = 0.045). No significant between-group difference in platelet count was found on days 14, 21 and 28 (P = 0.199; P = 0.253; P = 0.333). Peak platelet counts were recorded on the 14th day in group B (492 x 109/L), and on the 21st day in group A (536 x 109/L). A significant difference was obtained testing changes in platelet count at all time points observed within group A, and group B, respectively (P < 0.001). Post hoc testing showed significant increase in platelet count on day 7 compared to day 4 in group A, as well as on day 14 compared to day 7. No significant difference in platelet count was observed in the remaining monitoring days in group A (day 4 vs. day 1, day 21 vs. day 14, and day 28 vs. day 21). In group B, a significant decrease in platelet count was observed on day 4 compared to day 1, followed by a significant increase in platelet count on day 7 compared to day 4, as well as on day 14 compared to day 7. No significant difference in platelet count was observed in the remaining monitoring days in group B (day 21 vs. day 14 and day 28 vs. day 21).
Table 2. Platelet count in burn patient groups
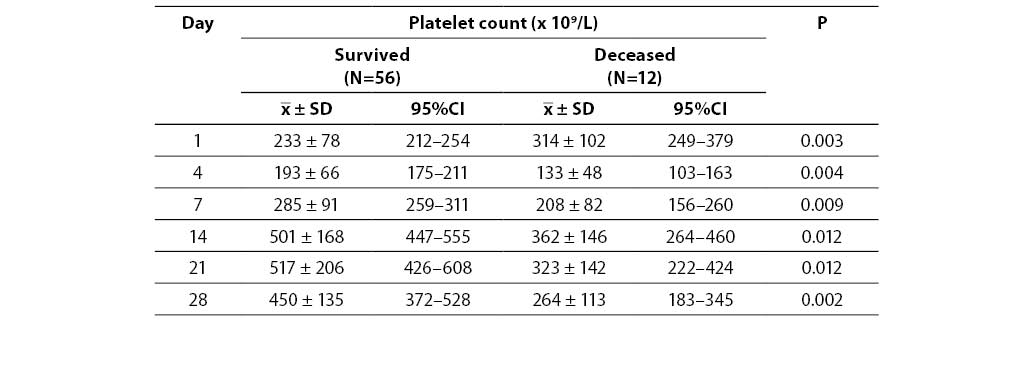
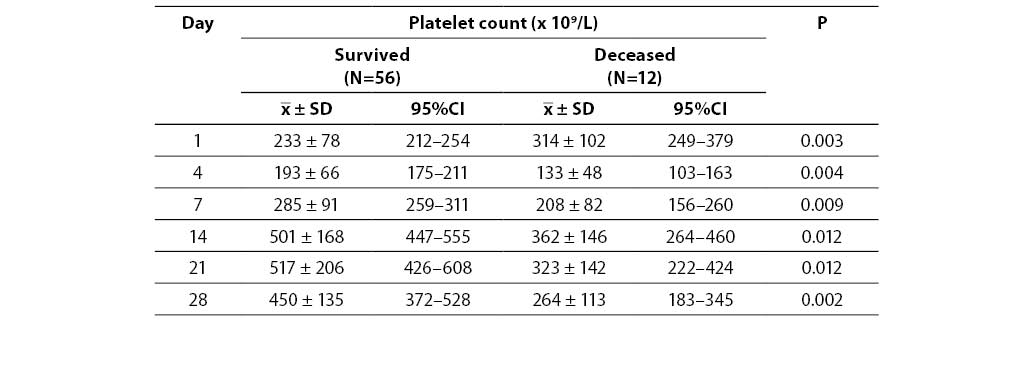
Platelet count according to disease outcome (survival/death) is shown in Table 3. A significant difference was found throughout the whole monitoring period by comparing surviving and deceased patients (P < 0.05). Significantly lower platelet count was observed in patients with lethal outcome on all monitoring days, except on day 1, when significantly higher platelet count was obtained compared to surviving patients. A significant difference was obtained testing changes in platelet count at all the time points in the surviving patient group, as well as within the group of deceased patients (P < 0.001). Post hoc testing showed a significant increase in platelet count on day 7 compared to day 4 in the surviving group, as well as on day 14 compared to day 7. No significant difference in platelet count was observed in the remaining monitoring days in survived patients group (day 4 vs. day 1, day 21 vs. day 14 and day 28 vs. day 21). A significant decrease in platelet count was observed on day 4 compared to day 1 in patients with lethal outcome. No significant difference in platelet count was observed in the remaining monitoring days in patients with lethal outcome (day 7 vs. day 4, day 21 vs. day 14, and day 28 vs. day 21).
Table 3. Platelet count in relation to disease outcome
Discussion
The results of this investigation revealed a significant difference in platelet count on the 4th and 7th day during monitoring in burn patient groups according to severity of injury; platelet count was lower in group B. A significant decrease in platelet count was observed in group B (moderate/severe burns) on day 4 compared to day 1, platelet count was below the reference range. A significant increase in platelet count was observed on day 7 compared to day 4 in both groups according to severity of burn injury. A rising platelet count tendency further continued on day 14 compared to day 7, but with no significant difference between groups.
Investigations dealing with time-dependent changes in platelet count in burn patients are rare. Takashima et al. recorded platelet count in five severely burned patients during clinical course after burn injury. They observed that platelet count decreased during 7-12 days, and after that stage numbers returned within the reference range or increased markedly. Platelet count stabilized just after two months (8). The time-dependent changes of platelet count in our investigation are similar to platelet count trend found by Sardaet al. (9) and Bartlett et al. (4). Bartlett and al. monitored coagulation and platelet changes in a group of 11 burn patients who manifested a progressive thrombocytopenia during the first three days after injury. Thrombocytopenia reached its maximum on the third day, the decrease being significant only in severely burned patients. Platelet count reached baseline values in the first week, followed by a reversal to abnormally high levels. In our investigation, a significant decrease in platelet count was observed only in the moderate/severe group of burn patients if day 4 was compared to day 1. Decrease in platelet count is caused by multiple and mostly interrelated factors. Platelet destruction is intensified, hemodilution is present, along with platelet sequestration (e.g., in the spleen) and their reduced production. A number of studies emphasize the relationship between thrombocytopenia in critically ill patients and platelet reduced life expectancy (10,11). Additionally, thrombocytopenia is frequently associated with bacterial sepsis present in these patients. In our investigation, a significant increase in platelet count was observed in both groups of patients on day 7 compared to day 4, and on day 14 compared to day 7, which can probably be explained by platelet contribution to the inflammatory reaction caused by burn injury. In fact, pathophysiological changes caused by burn injury are not localized to the site of burn injury, systemic inflammatory response results from the effects of released cytokines and endotoxins. An increase in platelet count represents normal response to a variety of inflammatory stimuli, whereas thrombocytopenia is considered to be an important issue concerning critically ill patients and is thought to play an important role in worsening the course of disease (12).
The percentage of TBSA, age and possible presence of inhalation injury are the major mortality determinants after thermal injury (3). Several investigations indicated the role of platelets as useful outcome indicators in burn patients (9, 13). Patients with lethal outcome followed up in our investigation were significantly older compared to surviving patients. A significant difference in platelet count throughout the entire monitoring period was observed in groups of patients according to disease outcome. Significantly lower platelet count was observed atall the monitored time points in patients with lethal outcome, except on day one when platelet count was significantly higher in this group of patients compared to those who survived. Higher platelet count in patients with lethal outcome on the 1st day can be caused by hemoconcentration. Furthermore, lower platelet count in patients with lethal outcome found in the remaining monitored days is probably caused by more serious burn injury and bacterial infection, theprocesses that stimulate thrombus formation in the coagulation cascade and intensive platelet consumption. Moreover, severity of injury and infection can depress bone marrow activity. El Sonbaty et al. (13) reported a significant platelet count increase on the 7th day in survivors after burn injury, while in those with lethal outcome a progressive decrease was recorded. In contrast, our results showed a platelet count increase in both groups in relation to disease outcome on the 7th day compared to the 4th day, but it was significant only in survivors.
We are aware of our study limitations: a limited number of investigated patients (especially in the group of patients with lethal outcome, and the group of mild burns where early hospital discharge was present), and on the other hand, unavailability of mean platelet volume (MPV) data, valuable for generating more complete information about the pathophysiological background of platelet count change at a given time point during monitoring of platelets in burn injury.
In conclusion, significant between-group differences recorded on the 4th and 7th day in groups of patients according to severity of injury, and significant decrease in platelet count recorded on the 4th day compared to the 1st day in moderate/severe burn patients in our study address the necessity for more frequent platelet count monitoring in this particular period of burn injury management in order to timely determine its decline. Significantly lower platelet count was observed throughout the whole monitoring period in patients with lethal outcome compared to survivors, except on day one, when platelet count was higher in this group. Despite the between-group differences in platelet count according to disease outcome, similar time-dependent changes in platelet count (increase and decrease) in both groups, and a limited number of study group patients, additional investigations are needed. Future investigations should address the usefulness of knowing platelet values and platelet curve monitoring in treatment, reducing the risk of complications during skin grafting, and disease outcome estimation.
Acknowledgements
We sincerely appreciate the technical support provided during this investigation by the staff of the Department of Burn Injury.
References
1. Kao CC, Garner WL. Acute burns. Plast Reconstr Surg 2000;105:2482-92.
2. Hettiaaratchy S, Dziewulski P. Pathophysiology and types of burns. BMJ 2004,328;1427-9.
3. Cakir B, Yegen BC. Systemic responses to burn injury. Turk J Med Sci 2004;34:215-26.
4. Bartlett RH, Fong SW, Marrujo G, Hardeman J, Anderson W. Coagulation and platelet changes after thermal injury in man. Burns 1980;7:370-7.
5. George NJ. Platelets. Lancet 2000;355:1531-9.
6. Klinger MHF. Platelets and inflammation. Anat Embryol 1997;196:1-11.
7. Weyrich AS, Lindemann S, Zimmerman GA. The evolving role of platelets in inflammation. J Thromb Haemost 2003;1:1897-905.
8. Takashima Y. Blood platelets in severelyinjured burned patients. Burns 1997;23:591-5.
9. Sarda DK, Dagwade AM, Lohiya S, Kamble AT. Evaluation of platelet count as a prognostic indicator in early detection of post burn septicaemia. Bombay Hosp J 2005;47(3). Aveilable at www.bhj.org., Accessed 25.01.2007.
10. Vaderschueren S, De Weerdt A, Malbrain M, Vankersschaever D, Frans E, Wilmer A, Bobbaers H. Thrombocytopenia and prognosis in intensive care. Crit Care Med 2000;28:1871-6.
11. Stephan F, Hollande J, Richard O, Cheffi A, Maier-Redelsperger M, Flahault A. Thrombocytopenia in surgical ICU. Chest 1999;115:1363-70.
12. Nijsten MWN, Duis HJ, Zijlstra JG, Porte RJ, Zwaveling JH, Paling JC, The H. Blunted rise in platelet count in critically ill patients is associated with worse outcome. Crit Care Med 2000;28:3843-6.
13. El-Sonbaty MA, El-Otiefy MA. Haematological change in severely burned patients. Annals of burns and fire disasters 1996;9(4):1-4.