Introduction
Note: part of this document has been endorsed as a Position Statement on Point of Care testing (in-hospital setting) of the Italian Society of Laboratory Medicine (Società Italiana di Medicina di Laboratorio, SIMeL). This document also refers to official documents and International standards to for generalities (ISO 15189/2003) (1) and specific items (ISO 22870/2006) (2); moreover it refers to professional standards, guidelines and peer reviews documents (3–8).
Up to the recent past years of the last millennium, a general trend commonly seen in most developed countries was to concentrate patients needing healthcare in structures of increasing complexity, starting from the Doctor Office up to the cottage hospital for the first basic aid and then to the large multi-specialty teaching hospitals for tertiary care. Yet, since then, multiple alerts of a different approach herald a possible inversion of this trend. The reasons for change can probably be found in the concurrent needs to reduce, on the one hand, the risk of dehumanization, incidental to many anonymous healthcare structures, and to relieve congestion in huge tertiary centers so to allow them a more efficient management of specialty cares. Laboratory Medicine Services are eliciting a similar trend: born at the bedside or as a ‘near-patient’ small office, migrated to separate locations, sometimes outside the hospital as for the reference laboratories. The increasing clinical impact of Laboratory Medicine finds its roots in a deeper understanding of pathophysiology of diseases, in a demand for a broader body of evidence for any medical action and on the overwhelming technological progress able to produce methods and devices with spectacular diagnostic sensitivity. Unfortunately, these exciting developments happen sometimes at cost of a holistic vision of the Patient and his/her own needs in favour of a pure technological approach. Moreover, the increasing, unavoidable process fragmentation in healthcare induced a huge rise of medical errors, and the resulting perplexities, criticism (or worse) in the Public. Today, the birth and development of diagnostic systems for Point of Care Testing (POCT) testifies that a paradigm shift has been occurring in Health Care: this offers a unique opportunity to bring back Laboratory Medicine once more ‘near the patients’ to help reducing the current fragmentation of care.
The Institute of Medicine (IOM) wishes a Healthcare System for the Millennium as:
1. safe – avoiding harm;
2. effective – evidence based;
3. patient centered – respectful of individual rights;
4. timely – to minimise delays;
5. efficient – able to avoid waste;
6. equitable – the same quality for everybody (9).
Laboratory Medicine can now guarantee for most tests performed as POCT the very same analytical quality as in central lab. Consequently, it offers a suitable platform to pursue the goals set by IoM. Still, Technology is not enough – per se – to meet two challenging demands:
- a whole system for Quality Assurance focused on the specific topic of instruments used by people with limited knowledge about In Vitro Diagnostics (IVD), or the patient
himself;
- a connectivity extended beyond the simple recording of patient data up to the full acknowledgment of the clinical meaning of a test result leading to the right decision and
subsequent medical action to be implemented.
No one of these crucial events should be taken for granted. Usually, in order to perform a lab test, you need to fulfil a minimum of 12 steps, or many more depending on the level of information technology used (requesting/releasing a test, sampleidentification, logistics, specimen receipt and handling). A vast majority of them could be avoided by adopting a POCT. By streamlining timing and analytical steps, one can focus just on the clinical question. Here lies the very cross-check of how correct was the choice to move on a POCT solution. The best possible outcome to be obtained in the care of the single patient is to maximize the benefits and minimize the risks without exceeding the boundaries of sustainable costs. The single stages where POCT is going to prove most useful are:
1. patient selection at the time of acute presentation and decision on immediate action;
2. treatment choice and optimization;
3. management of compliance;
4. patient (and physician) satisfaction, even about financial implications;
5. revenues for the payer.
Definitions
“Diagnostic system for POCT”: a Laboratory Medicine Service, with a specific Quality System, made of instrumentation + reagents + software + connectivity to the laboratory information system (LIS), suitable for the governance of the whole analytical process when performed ‘near patient’ instead of in the centralized Lab.
“POCT instrument”: analytical instrument specifically designed to perform in vitro diagnostic tests in the nearby of the patient (e.g., portable glucometers and coagulometers).
“POCT device”: any other resource (e.g.: reactive strips, immunocards, etc) used to gain information “near patient” about body constituents.
Note: here we intend to discuss about POCT systems inside the hospital. The general item of “decentralized diagnostics” is very much the same, but the possible practical applications differ significantly enough to justify a separate discussion.
Nowadays we can generate a lab test result at strict closeness to the patient, e.g. in the Emergency Room or a Paediatric Intensive Care Unit. In some circumstances, a fast result can help improving the clinical effectiveness, provided that it is reliable and accurate. This can explain the increasing popularity of POCT devices.
The goal is the proper use of POCT systems by trained personnel on the right patient in order to obtain results of good quality to insert into the patient file as clinically significant information. It is perhaps not redundant to state -once more- that a fast available result could be useful and effective only if accurate. Major risks derive from the limited competence of users, the lack of appropriate supervision/accreditation/ governance of POCT systems, the omitted use of quality assurance schemes or the improper performance by non expert staff and the uncertainties about a correct interpretation of results. In any case, it must be clearly stated that, today, POCT is by no means a surreptitious substitute for a clinical laboratory, rather an integration of its services.
True clinical governance is of paramount importance for POCT. The most practical tool to get it is the creation of a Multidisciplinary Steering Committee (MSC), usually chaired by a Pathologist, in charge of appraising the requests, establishing a priority scale and design the framework around the system in order to maximize the healthcare outcomes. The MSC will set up an Operational Team (OT) focused on the search of appropriate resources. A POCT Coordinator, usually a Medical Laboratory Technologist, is the pivotal role in this organization, wherein nurses must be fully involved. There should be suitable room for instruments, reagents and paperwork, OT and the coordinator oversee the daily routine, included the training program for the staff, the quality assurance and the performance appraisal, maintenance, supply storage and financial control, IT connectivity, health and safety. All processes should be collected and described as Standard Operational Procedures (SOPs). The MSC is responsible for decision on new tests/systems to be implemented on the basis of evidence of better medical outcomes.
Key aspects in developing a diagnostic system for POCT
1. An authoritative and pervasive clinical governance is mandatory – here more than wherever else- for any kind of POCT. The best way to get it is by means of a MSC, in which all the laboratory specialties involved should be represented.
2. The MSC, on behalf of the Institution, is in charge for the entire POCT system. It operates according to:
(a) relevant legislation (both National and European);
(b) Institutional and Laboratory accreditation standards;
(c) laws and restrictions in terms of data protection;
(d) risk management requirements.
3. Any request for POCT implementation should be evaluated based on the true clinical needs and the available resources, taking into account a maximum of quality goals measurable and attainable.
4. A POCT solution, no matter how sophisticated (from the single device up to complex integrated systems), should not be considered if the central lab can comply with the clinical situation.
5. A formal approval by MSC should be mandatory prior the introduction of any POCT device, regardless of the possible purchasing modalities (leasing, gift, tender).
6. An OT should be created to oversee the daily routine for POCT, with funding and facilities appropriate to the assigned tasks.
7. The Lab Director should be in charge of the global leadership and coordination of the activities and limitations related to POCT.
8. Any performed operation should be recorded as SOP according to manufacturer’s recommendations and professional standards.
9. Only staff whose training and competence has been established, recorded and regularly updated should be permitted to perform, maintain and supervise POCT.
10. Password protected access to the system should be only allowed to certified users.
11. Quality Assurance, in the widest meaning of the term, should be granted and monitored on a regular basis, since it is vital for POCT.
12. A full and effective connectivity should be implemented among the various system components and with the LIS. The best available technology should be used.
13. A procedure intended for the detection and reporting of any adverse event related to the practice of POCT should be in place.
14. The MSC should regularly review and check the previously defined quality goals.
15. The MSC is given the authority to suspend and repeal the service, wholly or partially, due to security, reliability or clinical convenience.
In the last years many examples of POCT have been produced, both in a hospital setting (Blood gas analysis, electrolytes, lactate, intra-operative PTH, glucose, alcool, and drugs of abuse, urine, glycated haemoglobin, albumin, INR for OAT, Ovulation/pregnancy tests, Clamydia/HIV, fecal occult blood) and in a community setting (glucose, urine, INR for OAT, ovulation/pregnancy tests).
Benefits and no risks?
An undisputable merit ascribed to POCT is the ability to produce and release analytical results earlier and easier than before by reducing the turn around time (TAT). This clear benefit, though, has to be balanced against a number of several potential risks. Moreover, “the faster the better” does not represent one and for all the best choice in any setting: timeliness depends on the specific clinical situation to be managed. The final decision should be made striking a balance among all the possible aspects, case by case. Often, a careful analysis of the whole process will lead to maintain a centralized diagnostics rather than to implement POCT. As a rule of thumb, it should be accepted that POCT is redundant whenever the laboratory can release a result as timely as clinically required. Taking into consideration that POCT is usually much more expensive than a centralized structure, its abuse always implies cost increases, not to mention the staff, whose training and management is also expensive: strangely enough this item is often ignored when preparing in-hospital POCT budgets. So it is mandatory to demonstrate that cost increases are fully counterbalanced by a much more efficient use of limited healthcare resources. Today, by virtue of spectacular progress in technology and detailed standards and regulations, POCT is much safer than a (even recent) past. Still, potential risks remain: staff with inadequate training, insufficient supervision, and lack of system governance and accreditation schemes. Again, it should be firmly stated that POCT can never be considered equivalent, rather an additional tool, for a clinical laboratory.
POCT implementation
POCT devices are used to perform analyses from a pre-defined test menu drawn up in agreement with clinicians on the basis of true medical needs when appropriate resources (in terms of technology, management, communication) are available. Each device should be allocated into an institutional ‘POCT system’ managed by a MSC. An OT should attest that responsibilities are clearly defined and largely known and should offer support and advice in appraising and selecting each device. The central laboratory should activate and manage the POCT system by:
- assessment of new technology and appropriate comparison among different solutions;
- protocols and procedures shared with all stakeholders;
- setting up an OT is the preliminary step needed to create a multi-professional, multi-disciplinary team led by a POCT Coordinator, including clinical staff (doctors and
nurses), engineers, clerks and, compulsorily, lab technologists;
- the Lab Director should lead the MSC being in charge of the whole organization and of the final decision about the implementation of any new device, instrument or system.
All the documents should be compiled according to the standards of UNI EN ISO 9000/ISO 15189 and 22870 and any other regulation, instruction, quality definitions. It is also advisable to keep records of installation date, trial and maintenance of each system component by the staff and by the manufacturer. A register containing all this files should be kept by the Clinical Engineering Service. Whenever possible, set up a dedicated software readily available (e.g. by the hospital intranet). The real time recording of the maintenance events allows a fast detection for any “drift” in users’ behaviour making it possible to schedule supplementary training sessions. Training for POCT users: it should be compulsory a certified attendance to dedicated courses with regular updates. Better still; a personalized format should be available, based on the actual system utilization by the single operator.
The analytical Quality control must be absolutely consistent with the traditional schemes of statistical QC adopted by the central lab. “Alternative” control schemes should be carefully appraised and appropriately confirmed by scientific and experimental evidence; however they do not cancel, decrease or limit, under any circumstance, the full responsibility of the Laboratory as far as Quality Assurance of POCT system is concerned. QC procedures should be meticulously described in specific SOPs. There should be room for a detailed description of responsibilities (lab, wards, and clinical services), procedures (materials, analytical levels, frequency) and EQA, provided that a reliable scheme be available.
Users’ safety: according to in force regulations on workplace safety is under the responsibility of the Laboratory. Instrument choice, adequate training and related themes should be discussed in specific training sessions.
How to implement an in-hospital POCT system
First and foremost, the set up of a MSC, appointed by the top Management of the Institution to whom devolve power for:
1. sharing the project with all stakeholders;
2. representing in full the Authority presiding over the in-hospital POCT system;
3. defining competences and responsibilities for each component inside the project;
4. defining criteria for preliminary choices before starting with POCT;
5. carefully appraising the available resources;
6. selecting wards/services where POCT devices are to be placed;
7. selecting a test menu;
8. activating a regular scheme of clinical audit about the appropriateness of the whole organization in order to check:
9. system effectiveness, based on measurable outcomes;
10. system soundness;
11. evaluating on a regular basis the global cost/effectiveness;
12. planning continuous quality improvement of the system.
Proposal
When applying for a test to be performed at POC, an evidence based pathway should be covered, aiming to meet the following items:
1. An answerable clinical question: A clear definition of the informative gap to bridge by performing that specific test in the context of the clinical presentation.
2. What clinical decision based on the test result: The relevance of a fast release of a result to make appropriate decisions (ruling in/ruling out).
3. What action to implement based on the test result: Possible use of drugs (including blood derivatives) in order to gain patient stabilization; patient access to further (invasive) diagnostics; patient discharge.
4. Expected benefits: Time optimization of patient journey, reduction of resources’ waste, operators’ confidence and reliability, patient satisfaction.
5. TAT needed: Total turn around time, therapeutic turn around time (tTAT) related to true clinical needs; tTAT reduction and associated improvements in cost/benefit (Length of stay in ED, lesser use of unnecessary resources).
6. Why the Lab can not meet the request: Test number, time to test release; disadvantages/infeasibilities of a central lab performance; IT connectivity.
7. Adequate precision/accuracy: Analytical performances should be consistent and meet the clinical question in a reliable and reproducible way even when compared with the same test as performed by the central lab; MSC is entitled to guarantee the global quality of decentralized tests performed inside the institution. A Quality control scheme should be in place for each instrument and test; quality standards should be comparable to traditional QC procedure, performed on a regular basis, by traceable material; a track should be kept of any corrective action made; a definite correlation with homologous performances by the central lab is required
8. Staff:It should be adequate in number to comply with organizational needs; an appropriate and traceable training program compulsorily updated should be in place for any POCT user; support should be granted by lab personnel when inadequate performances occur
9. Resources
10.Training: In addition to the analytical phase, information should be given about pre-analytical variables, quality control and its statistical rules, and post-analytical factors with special focus on reporting; only trained personnel, regularly kept up to date, is entitled to access POCT system; the training program should be supervised and updated by the POCT Coordinator and by the Lab Director
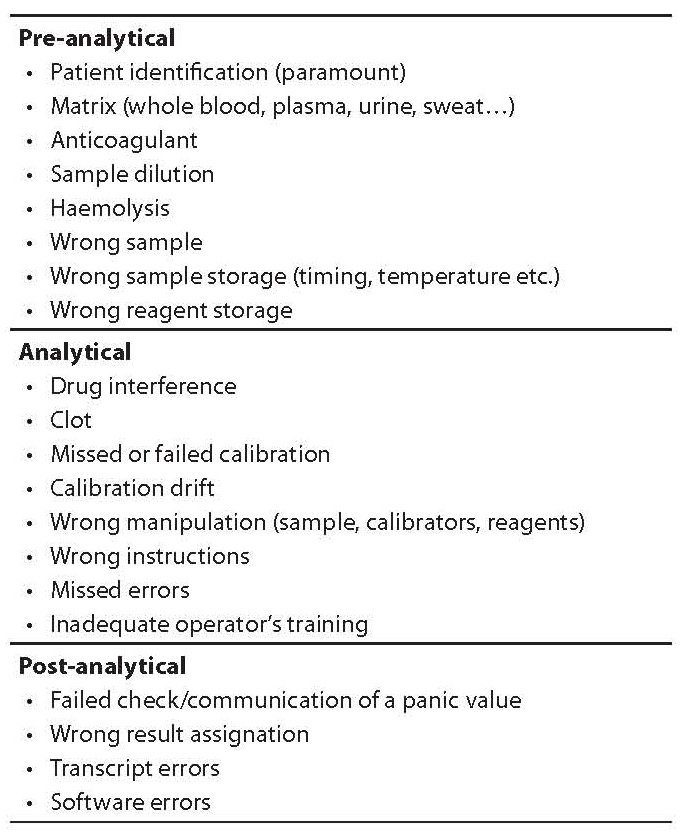
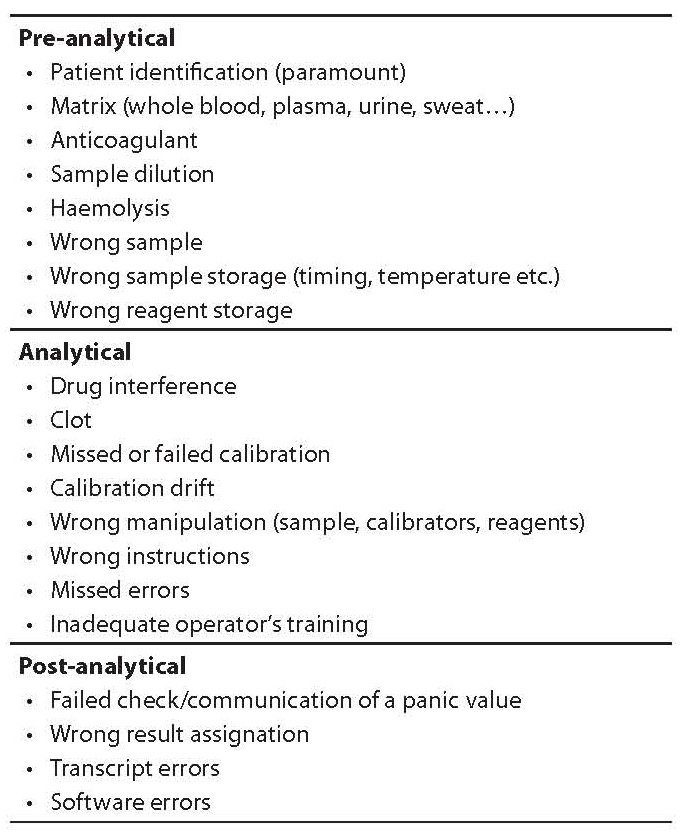
Main sources of errors
From the analytical side, all efforts should be granted to look for the best possible test precision and accuracy, by means of a pervasive QC and Quality Assurance. The nature and distribution of errors is well known in Laboratory Medicine, since the processes are firmly structured and related to precise and internationally accepted standards. The pre-analytical phase includes patient preparation. To improve the post-analytical phase a close cooperation in managing the report and a special focus should be placed on its best use (interpretative comments, advice, measure of outcomes and audit trail), as also required by international standards (Table 1).
Table 1. Main sources of errors in point of care testing (POCT).