Serum cholesterol concentration in psychiatric patients
Nedjeljka Ruljančić
[*]
[1]
Ana Malić
[1]
Mate Mihanović
[1]
Introduction
In modern medicine, interest has long been focused on the association between serum cholesterol concentration and suicide, the latter posing a major problem in the management of psychiatric patients. An increased incidence of suicidal deaths was recorded in subjects included in clinical trials of cholesterol lowering drugs (1). Serum cholesterol has thus incidentally become a topic of research as a biological risk factor in individuals dying a violent death. Indeed, many subsequent studies found low serum cholesterol to be a risk factor for suicide (2-4), while others failed to confirm the hypothesis (5,6). The neurobiological aspect of suicide has also been extensively investigated.
Cholesterol is found in the central nervous system (about 20%) and is also involved in cell structure and its function. The mechanism by which low cholesterol concentration might be associated with cerebral function has not yet been clarified. There are numerous hypotheses, one of the most frequently cited ones being that proposed by Engelberg (1992), that low serum cholesterol concentration leads to a decreased cerebral concentration of cholesterol, thus reducing the cholesterol content in brain cells (glial cells, neurons, astrocytes). Low cholesterol has been postulated to reduce the activity of serotonin receptors and serotonin transporter due to a decreased lipid microviscosity of neuronal membrane because it increases the neuronal cell membrane fluidity (7). However, not all studies demonstrated such changes associated with low cholesterol concentration. The more so, an enhanced activity of serotonin transporter and a consequentially increased serotonin uptake have been reported (8). Other possible mechanisms have also been studied, e.g., modulation of the serotonin receptor function and cholesterol involvement in the synapse formation (9-11). Accordingly, it is concluded that cholesterol has different roles in different directions of synaptic transmission, i.e. via neurotransmitter system modulation by change in membrane fluidity, or direct molecular interaction or regulation of synaptogenesis.
The considerable interest in the postulated association between serum cholesterol and suicidal attempts, and the controversial evidence found in the literature stimulated the present study aimed at assessing the possible variation in serum cholesterol concentration among patients with different psychiatric diagnoses.
Materials and methods
Patients
All patients admitted to Sveti Ivan Psychiatric Hospital from January 1, 2005 till April 1, 2005, were included in the study. Patients with psychiatric diagnoses of low prevalence were not included. In a total of 677 patients, fasting blood samples were collected during routine work-up on the second day of admission. Patients were divided into nine groups according to the International Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) (12): F10 dependence syndrome (alcoholism, illicit drugs, drugs); F20 schizophrenia; F23 psychotic disorder; F25 schizoaffective disorder; F32 depressive disorder; F43 stress reaction (acute, posttraumatic); F60 personality disorder (paranoid, dissociative, emotional); X61 nonviolent suicidal attempt (drug poisoning); and X70 violent suicidal attempt (hanging, suffocation, sharp object). There were 262 female and 415 male patients aged 17-89.
Blood samples were collected after psychiatric examination, according to standardized procedure and in line with ethical principles (with approval issued by the Hospital Ethics Committee).
Methods
Total serum cholesterol concentration was determined by the standard CHOD-PAP method on a Roche Diagnostics Cobas Integra 400 biochemistry analyzer and reagents from the same manufacturer.
Statistical analysis
Collection of data for statistical analysis was performed by use of the Microsoft Office Excel 2000 software (Microsoft, USA). Descriptive statistics was performed for all the variables analyzed. Variance homogeneity was tested by Bartlett test and cholesterol distribution normality according to groups by Kolmogorov-Smirnov test. As the test of variance homogeneity proved satisfactory, between-group differences in cholesterol concentration were tested by the ANalysis Of VAriance (ANOVA) test, while multiple LSD post hoc test was employed to identify the groups yielding this difference. In all analyses, the level of significance was set at 5%. All analyses and graphic presentation were done by use of STATISTICA 7.1 statistical package.
Results
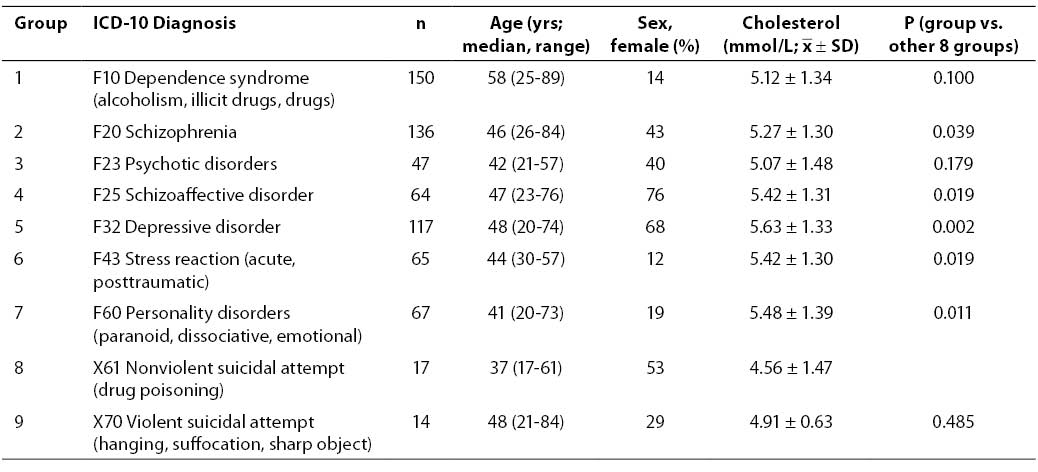
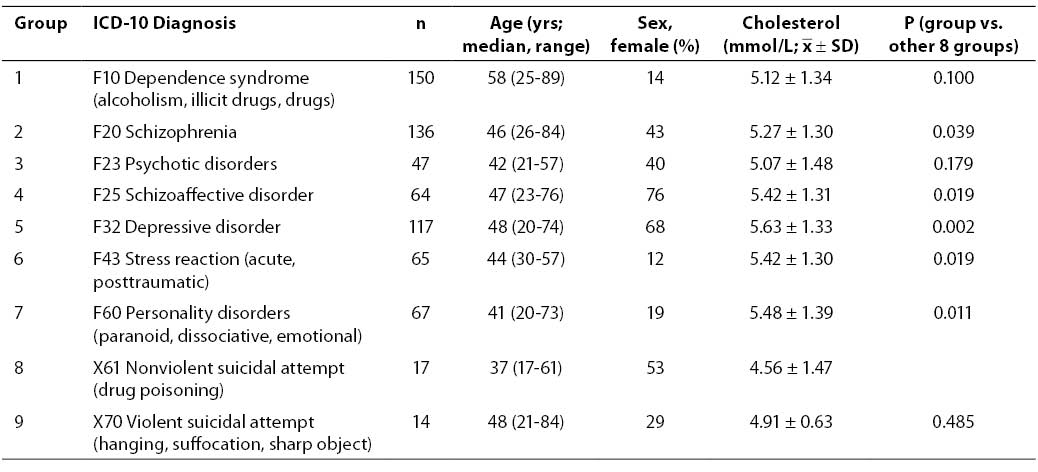
Study results showed the concentration of serum cholesterol to vary among the groups of patients with different psychiatric disorders. Generally, patients with a history of attempted suicide had a lower level of serum cholesterol than other patient groups, with the lowest level measured in patients with the diagnosis of nonviolent suicidal attempt (X61). Differences in serum cholesterol concentration among patient groups with particular diagnoses were estimated by ANOVA because the test of variance homogeneity showed no statistically significant variance differences (P = 0.19). Analysis of variance yielded a statistically significant difference among the groups of patients with different diagnoses (P = 0.012). Multiple post hoc test (LSD) revealed the group of patients diagnosed with X61 to differ statistically significantly from the groups of patients diagnosed with schizophrenia (F20) (P = 0.039), schizoaffective disorder (F25) (P = 0.019), depressive disorder (F32) (P = 0.002), stress reaction (F43) (P = 0.019) and personality disorder (F60) (P = 0.011), which all had higher serum cholesterol levels (Table 1).
Table 1. Total serum cholesterol concentration in nine patient groups according to ICD-10 classification (ANOVA, P=0.012)
Discussion
The present study demonstrated statistically significant differences in serum cholesterol between nonviolent suicide attempters and all other psychiatric patients diagnosed with F20, F25, F32, F43 and F60. Serum cholesterol concentration was lower in the former (4.56 ±1.47 mmol/L). The group of violent suicide attempters also had lower serum cholesterol, however, the difference from the group of nonviolent suicide attempters did not reach statistical significance (P = 0.485). These results are in contrast to those reported from other studies where violent suicide attempters were found to have a statistically significantly lower serum cholesterol in comparison to nonviolent suicide attempters (4,13,14). The absence of significant difference in serum cholesterol between the violent and nonviolent suicide attempters in our study may have been due to the small number of these patients (17 nonviolent and 14 violent suicide attempts). In addition, the mode of attempting suicide has been presumed to be determined by the availability of some external factors for the particular type of suicide (15). This concept would decrease the potential role of biological factor and may explain the lack of difference in cholesterol level between our patient groups of violent and nonviolent suicide attempters. Interesting results were observed in the group of patients with depressive disorder, where the highest serum cholesterol level was measured (5.63 ±1.33 mmol/L). This finding was inconsistent with other literature reports on a strong correlation between depression and low serum cholesterol (16-18), implying suicidal behavior in these patients.
The present study probably suffered from some limitations because we did not explore the potential psychiatric history of suicide attempters, which may have revealed coexistence of some other psychiatric disorders. In this way, the information on suicidal behavior and on the cholesterol level indicative of such behavior would be by far more exact. We are also aware of the study limitation due to the lack of data on body mass index (BMI), as the increase in BMI has been demonstrated to reduce the risk of suicide (19). An increased suicidal behavior could be assumed in patients with dependence syndrome (alcoholism, illicit drugs, drugs) (F10) and psychotic disorder (F23), since there was no statistically significant difference in serum cholesterol in comparison with nonviolent suicide attempters (in these groups, serum cholesterol concentrations were quite comparable). As alcohol dependence poses a risk of suicide (20), serum cholesterol concentration has already been investigated in subjects suffering from this psychiatric disorder; however, no overt association was found between serum cholesterol and suicide attempts (21). Our results are consistent with the lower cholesterol level recorded in cocaine abusers, demonstrated to be predictive of cocaine dependence relapse (22).
The statistically significant difference in serum cholesterol levels between the group of nonviolent suicide attempters and groups of patients diagnosed with F20, F25, F43 and F60, which showed statistically significantly higher serum cholesterol, appears to suggest that lowering serum cholesterol may imply the risk of suicidal behavior in these patients.
Additional studies should include serum cholesterol monitoring over a longer period in all groups of psychiatric patients, on the model of long-term follow up studies of risk factors for coronary disease conducted in healthy subjects, which found a low cholesterol concentration and cholesterol concentration declining over years to be associated with an increased risk of death from suicide (23). Accordingly, cholesterol concentration could be used as a factor of predisposition for suicidal behavior, thus contributing to the prevention of suicide in psychiatric patients.
Acknowledgment
The authors are thankful to Ana-Marija Jazbec, PhD, for her valuable assistance in statistical data processing.
References
1. Muldoon MF, Manuck SB, Matthews KA. Lowering cholesterol concentrations and mortality: a quantitative review of primary prevention trials. BMJ 1990;301:309-14.
2. Partonen T, Haukka J, Virtamo J, Taylor PR, Lonnqvist J. Association of low serum total cholesterol with major depression and suicide. Br J Psychiatry 1999;175:259-62.
3. Golier JA, Marzuk PM, Leon AC, Weiner C, Tardiff K. Low serum cholesterol level and attempted suicide. Am J Psychiatry 1995;152:419-23.
4. Garland M, Hickey D, Corvin A, Golden J, Fitzpatrick P, Cunningham S et al. Total serum cholesterol in relation to psychological correlates in parasuicide. Br J Psychiatry 2000;177:77-83.
5. Tanskanen A, Vartiainen E, Tuomilehto J, Viinamaki H, Lehtonen J, Puska P. High serum cholesterol and risk of suicide. Am J Psychiatry 2000;157:648-50.
6. Almeida-Montes LG, Valles-Sanchez V, Moreno-Aguilar J, Chavez-Balderas RA, Garcia-Marin JA, Cortes Sotres JF et al. Relation of serum cholesterol, lipid, serotonin and tryptophan levels to severity of depression and to suicide attempts. J Psychiatry Neurosci 2000;25:371-7.
7. Engelberg H. Low serum cholesterol and suicide. Lancet 1992;339:727-9.
8. Vevera J, Fišar Z, Kvasnička T, Hanuš Z, Starkova L, Češka R et al. Cholesterol-lowering therapy evokes time-limited changes in serotonergic transmission. Psychiatry Research 2005;133:197-203.
9. Lalović A, Levy E, Luheshi G, Canetti L, Grenier E, Sequeira A et al. Cholesterol content in brains of suicide completers. Int J Neuropsychopharmacol 2007;10(2):159-66.
10. Lalovic A, Sequerira A, DeGuzman R, Chawky N, Lesage A, Seguin M et al. Investigation of completed suicide and genes involved in cholesterol metabolism. J Affect Disord 2004;79:25-32.
11. Mann JJ, Brent DA, Arango V. The neurobiology and genetics of suicide and attempted suicide: a focus on the serotonergic system. Neuropsychopharmacology 2001;24(5):467-77.
12. Svjetska zdravstvena organizacija. Međunarodna klasifikacija bolesti i srodnih zdravstvenih problema (MKB-10). 10. revizija, Svezak 1. Zagreb: Medicinska naklada; 1994.
13. International classification of diseases and related health problems, Tenth Revision (ICD-10). Vol. 1. Zagreb: Medicinska naklada; 1994.
14. Vevera J, Zukov I, Morcinek T, Papezova H. Cholesterol concentrations in violent and non-violent women suicide attempters. Eur Psychiatry 2003;18:23-7.
15. Marčinko D, Martinac M, Karlović D, Filipčić I, Lončar Č, Pivac N et al. Are there differences in serum cholesterol and cortisol concentrations between violent and non-violent schizophrenic male suicide attempters. Coll Antropol 2005;29(1):153-7.
16. Mann JJ. Neurochemical studies of violent and nonviolent suicide. Psychopharmacol Bull 1989;25:407-12.
17. Morgan RE, Palinkas LA, Barrett-Connor EL, Wingard DL. Plasma cholesterol and depressive symptoms in older men. Lancet 1993;341:75-9.
18. Suarez EC. Relation of trait depression and anxiety to low lipid and lipoprotein concentrations in healthy adult women. Psychosom Med 1999;61:273-9.
19. Steegmans PHA, Hoes AW, Bak AAA, van der Does E, Grobbee DE. Higher prevalence of depressive symptoms in middle-aged men with low serum cholesterol levels. Psychosom Med 2000;62:205-11.
20. Magnusson PKE, Rasmussen F, Lawlor DA, Tynelius P, Gunnell D. Association of body mass index with suicide mortality: a prospective cohort study of more than one million men. Am J Epidemiol 2006;163:1-8.
21. Rossow I, Romelsjo A, Leifman H. Alcohol abuse and suicidal behavior in young and middle aged men: differentiating between attempted and completed suicide. Addiction 1999;94:1199-207.
22. Deisenhammer EA, Lechner-Schoner T, Kemmler G, Ober A, Braidt E, Hinterhuber H. Serum lipids and risk factors for attempted suicide in patients with alcohol dependence. Alcohol Clin Exp Res 2006;3(3):460-5.
23. Buydens-Branchey L, Branchey M. Association between low plasma levels of cholesterol and relapse in cocaine addicts. Psychosom Med 2003;65:86-91.
24. Zureik M, Courbon D, Ducimetiere P. Serum cholesterol concentration and death from suicide in men: Paris Prospective Study I. BMJ 1996;313:649-51.