Introduction
Sample hemolysis is universally regarded as a major challenge for the quality of diagnostic testing. Despite a final diagnosis of hemolytic anaemia can only be established in a minority of patients, in vitro hemolysis is the underlying cause of the vast majority of hemolysed samples received in clinical laboratories (1). The prevalence of hemolysed specimens is particularly high in those healthcare settings where blood is drawn from intravenous lines (2), which typically include short stay units such as the emergency department (ED), intensive care units, paediatric and oncology wards. In the ED, in particular, the rate of hemolysed specimens has been reported as high as 12% (1).
Due to the high prevalence of hemolysis in samples received from the ED, several strategies were proposed to overcome the problem (3). The use of traditional means of collection other than drawing blood from intravenous lines has been widely advocated (4), but this suggestion has been largely overlooked due to the fact that blood drawing from catheters is thought to save time as well as human and economical resources that are required for both patient care and blood drawing in short stay units. The effectiveness of using low volume tubes is also questionable, since the use of these devices reduced the burden of spurious hemolysis in some facilities (5), but not in others (6), and the different outcome has been attributed to the different study population and the use of different types of tubes. The use of specific holders, such as those with an eccentric luer, was also helpful to reduce gross (i.e., cell-free haemoglobin > 3.0 g/L) but not mild (i.e., cell-free haemoglobin from 0.5 to 3.0 g/L) hemolysis (7).
Promising results were obtained in a preliminary study including 52 consecutive ED patients, when blood drawing using a conventional vacuum system was replaced with another primary closed collection system based on manual aspiration of blood (S-Monovette, Sarstedt AG & Co., Nümbrecht, Germany) (8). More specifically, the use of the S-Monovette system in the aspiration mode was effective to reduce the rate of hemolysed samples collected from intravenous lines by approximately 27% when compared with a traditional vacuum system. Therefore, the aim of this observational study was to verify whether the routine replacement of a conventional vacuum system with the S-Monovette system may be effective to reduce the burden of hemolysis in the daily practice of a large urban ED.
Materials and methods
Study design
This study was based on the systematic identification of hemolysis in serum samples received in the clinical laboratory of the University Hospital of Parma from the local ED, a large urban facility with approximately 92.000 visits per year. In this ED, blood samples are typically drawn using intravenous catheters (1.0 x 3.2 mm, 20-gauge catheter; Neo DELTA VEN, Viadana, MN, Italy). According to the study protocol, the investigation was divided in two observational periods of 4 months each.
In the former period (i.e., from the 1st of January to the 30th of April, 2014), blood was collected from intravenous catheters using 13x100 mm x 5.0 mL BD Vacutainer® SST II Plus plastic serum tubes (Becton Dickinson Italia S.p.A, Milan, Italy). According to the positive outcome of a previous local investigation (8), the Direction of the University Hospital of Parma authorized the complete replacement of these serum tubes with 4.0 mL S-Monovette serum tubes (S-Monovette, Sarstedt AG & Co., Nümbrecht, Germany) on May 15th, 2014. After 15 days of familiarization with the new blood collection device, the second observational period started on the 1st of June, 2014, and was concluded on the 30th of September, 2014. In this second phase of the study, blood was collected from intravenous catheters by the ED personnel always using S-Monovette blood tubes in aspiration mode.
Methods
During both phases of the study, sample hemolysis was systematically assessed on all serum samples received from the local ED by photometrical measurement on a Beckman Coulter AU5800 (Beckman Coulter Inc., Brea, CA, USA). In this instrument the hemolysis index is quantified by bichromatic readings at 410/480 and 600/800 nm, providing semi-quantitative levels of cell-free haemoglobin from 0 to 5 g/L. The conventional criterion used in our laboratory for considering a serum sample as hemolysed is the presence of ≥ 0.5 g/L of cell-free haemoglobin in serum, in agreement with current recommendations (9).
The data of all hemolysed specimens received in the laboratory, including those from the ED, were systematically entered into software specifically designed for recording preanalytical non conformities (10). The personnel of the ED, as well as the local practice for sample handling, transportation, preparation and analysis were not changed throughout the two study periods. Moreover, the ED and the laboratory are located in the same building, with a common air conditioning system that maintains stable conditions of temperature and humidity regardless of the external environmental condition. The study was carried out in accordance with the Declaration of Helsinki and under the terms of all relevant local legislations.
Statistical analysis
The statistical analysis was based on Chi-squared statistics with Yates’s correction, using Analyse-it (Analyse-it Software Ltd, Leeds, UK) and the statistical significance was set at P < 0.05.
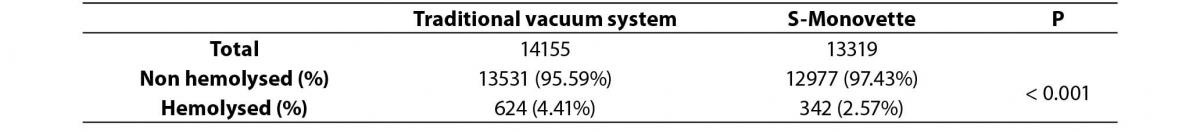
Table 1. Hemolysis rate in serum samples collected from intravenous lines in the emergency department with a traditional vacuum system and with the S-Monovette blood drawing system in aspiration mode.
Results
The total number of serum blood tubes received in the laboratory from the ED was 14,155 in the former phase of the study, whereas 13,319 serum tubes were received in the second phase of the study. The total number of hemolysed serum specimens was 624 in the first phase of the study, and 342 in the second phase of the study, respectively. Accordingly, the hemolysis rate was 4.41% using the conventional vacuum system, but decreased by nearly a half using S-Monovette serum blood tubes in aspiration mode (2.57%; Chi-squared statistics, 67.98; P < 0.001) (Table 1).
Discussion
Spurious hemolysis in samples collected in the ED remains a major healthcare problem, since it consumes precious human and economical resources, but also jeopardizes patient safety when unreliable results obtained on hemolysed samples are reported to the requesting physician (1). We have previously shown the use of S-Monovette system in the aspiration mode was effective to reduce hemolysis in samples drawn from intravenous catheters. More specifically, in a prospective, randomized study including a limited number of patients (N = 52), we showed that the concentration of potassium, lactate dehydrogenase and cell-free haemoglobin was significantly reduced when samples were collected with S-Monovette system in the aspiration mode compared to conventional vacuum tubes (8). The promising data emerged from this preliminary investigation persuaded the Direction of our University Hospital to completely replace the use of the former conventional vacuum system with S-Monovette blood tubes for routine blood collection in the ED. Interestingly, the results of the present observational study confirm that this strategy was effective to reduce the burden of hemolysed specimens in the ED compared to the use of a conventional vacuum system such as Vacutainer® SST II Plus plastic serum tubes. More specifically, the hemolysis rate was decreased by nearly a half after introduction of the novel blood drawing system (i.e., from 4.41% to 2.57%). This important outcome is probably attributable to the fact that the manual aspiration of blood within a closed system such as S-Monovette may consistently reduce the shear stress and the consequent injury of blood cells compared to the forced aspiration that characterizes the conventional vacuum system (8). More specifically, this device may be used as a standard primary collection system, and the vacuum can be generated before sample collection by locking the piston into the base of device and breaking off the plunger. Alternatively, S-Monovette can also be used as a syringe, since blood can be aspirated into the tube by slow withdrawn of the plunger until tube filling is completed. A potential limitation of this study is represented by the fact that we used two different observational periods (i.e., January-April and June-September), so that we cannot rule out that a heterogeneous disease spectrum may have occurred in the ED.
Nevertheless, we believe that these results may have meaningful implications under a clinical and organization perspective, since a second venipuncture for obtaining a suitable serum sample for laboratory testing could be avoided in as many as 1.8% of the patients. This may be clearly associated with a significant saving of economical (i.e., additional blood tubes and labels) and human resources in the increasingly overcrowded environment of an ED. Even more importantly, the ED stay and the final time for diagnosis may also be reduced due to elimination of the diagnostic delay attributable to the need of sample recollection when the former diagnostic specimen is hemolysed.
Conclusion
Results of our study confirm that the introduction of the Sarstedt S-Monovette blood tubes has reduced the hemolysis rate in the emergency department compared to the previously used BD Vacutainer® SST II Plus plastic serum tubes.


