Introduction
Heart failure (HF) is a condition in which the heart cannot pump sufficient oxygenated blood to meet the metabolic needs of body tissues (1). Although HF is a chronic disease, many patients experience acute symptoms, resulting in visits to the emergency department (ED). Specific mechanisms leading to the development of acute heart failure (AHF) and the adverse outcomes associated with it remain unclear (2).
B-type natriuretic peptide (BNP) is a cardiac hormone mainly secreted by cardiac myocytes in response to ventricular volume expansion, pressure overload, and resultant increased wall tension (3). BNP concentration in blood is a sensitive and specific test for the identification of heart failure patients presenting with acute dyspnea to the emergency department (1,4). Moreover, a BNP concentration cutoff of 100 ng/L may be useful in distinguishing between cardiac and noncardiac causes of acute dyspnea (1,4). BNP concentrations also correlate with the severity and prognosis of illness (5).
Mean platelet volume (MPV), a routine measure of platelet size, may reflect increased platelet activation or increased numbers of large, hyperaggregable platelets (6). MPV levels were recently shown to be increased in a number of disease states, including myocardial infarction, unstable angina, and stroke (6,7). In addition elevated MPV was shown to be an independent risk factor associated with adverse cardiovascular events (8). Although recent studies have shown increased platelet activation in patients with heart failure (6), current evidence is insufficient to support the hypothesis that platelet activation plays a direct role in the pathophysiology of AHF. It is unclear whether increased platelet activity is related to a systemic imbalance or actually contributes to acute decompensation.
To our knowledge, no study to date has evaluated the relationship between BNP concentrations and MPV in patients with AHF. This study therefore retrospectively compared MPV levels and total thrombocyte counts in patients with and without AHF and the correlations of these factors with BNP, as well as with total white blood cell (WBC) count and neutrophil–lymphocyte (N/L) ratio as indicators of systemic inflammation.
Materials and methods
Study design
This retrospective cohort study utilized hospital databases data from 319 patients admitted to the Emergency department of Bursa Yüksek İhtisas Research and Education Hospital from January to July 2014. The study was approved by the institutional ethics committee of the hospital and was in compliance with the Helsinki Declaration.
Subjects
Eligible patients were identified by a review of computer-based clinical records. Patients presenting with acute dyspnea as their main symptom and diagnosed with AHF according to European Society of Cardiology criteria were recruited (1). AHF as the leading diagnosis was the only inclusion criterion (i.e., patients with acute coronary syndrome as the main diagnosis were not included). All records were reviewed for confirmation of diagnosis, but none was excluded.
The control group consisted of patients who presented with shortness of breath as their primary complaint and had no obvious traumatic or infectious cause of dyspnea. Patients with severe renal disease (serum creatinine > 250 μmol/L) and patients in cardiogenic shock were excluded.
Methods
EDTA blood samples (BD Vacutainer K2EDTA Plus plastic tubes; Becton Dickinson, Franklin Lakes, NJ, USA) were drawn from each patient at the time of admission and, according to the protocol of our emergency department, processed within 30 minutes of venipuncture. Samples were analyzed in an automated hematology analysis system (Coulter LH-780 hematology analyzer; Beckman Coulter Inc., Fullerton, CA, USA), which measures platelet size and platelet count using aperture-impedance technology.
BNP concentrations were measured quantitatively using a fluorescence immunoassay with a single use device (Triage BNP Test; Biosite Inc., San Diego, CA) (8). The assay procedure involved the addition of several drops of an EDTA whole blood specimen to the sample port on the test device. A filter separated the red blood cells from plasma and the plasma moved by capillary action into a reaction chamber to form a reaction mixture. After the incubation period, the reaction mixture flowed through the device detection lane, with complexes of BNP and fluorescent antibody conjugates captured in a discrete zone of the detection lane. The concentration of BNP in the specimen was proportional to the fluorescence bound in the detection lane and was quantified by the portable triage meter. The analytical characteristics of the system have been described previously; the intraassay and interassay coefficients of variation (CV%) of these kits were 8.8–11.6% and 9.9–12.2%, respectively. (9). BNP concentrations were measured within 30 minutes of venipuncture.
Statistical analysis
All statistical analyses were performed using SPSS 10.0 (SPSS for Windows 10.0, Chicago, IL,USA). Statistically significant differences between parameters with a Gaussian distribution were analyzed using Student’s t-tests and variables with a non-Gaussian distribution were compared using the Mann-Whitney U test. Normal distribution was assessed using the Kolmogorov-Smirnov test. Correlations were analyzed using Spearman’s correlation test. Continuous variables are expressed as mean ± SD. All P values were two-sided, with a P value < 0.05 considered statistically significant.
Results
The study included 190 patients admitted to the emergency department with AHF and 129 without AHF. Demographic, clinical and laboratory parameters in the two groups are presented in Table 1. BNP concentrations in patients with and without AHF were 200-5000 ng/L and 5-98 ng/L, respectively. MPV levels (P < 0.001), total neutrophil counts (P = 0.001) and neutrophile / lymphocyte ratios (P = 0.001) were significantly higher in the AHF than in the control group.
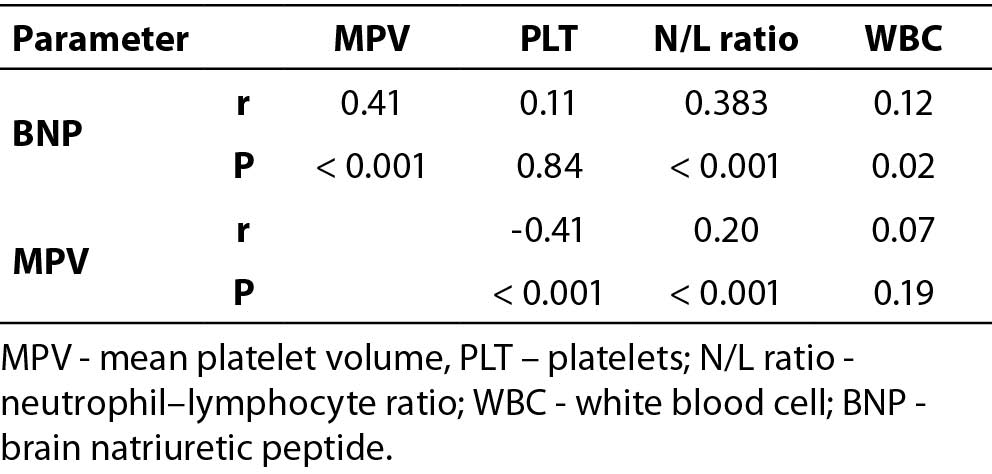
Data from the two groups were pooled to analyze the relationships between BNP and MPV, and with other hematological parameters (Table 2). BNP concentration was positively correlated with MPV (r = 0.41, P < 0.001) and PNL/L ratio (r = 0.38, P < 0.001).
There was a weak, although significant, negative correlation between MPV and platelet count (r = −0.41, P < 0.001).
Discussion
Although platelet numbers was similar in patients with and without AHF admitted to the emergency department, MPV was significantly higher in patients with AHF. Previous studies have assessed the prognostic role of MPV in patients with cardiovascular diseases, although the mechanism responsible for increased platelet size in these patients remains unclear (10). MPV appears to correlate more closely with platelet function than does platelet count alone (6). Large platelets that contain more dense granules are metabolically and enzymatically more active than small platelets and have higher thrombotic potential. Platelet abnormalities described in patients with chronic heart failure (CHF) and AHF include increases in P-selectin expression, platelet aggregation, the expression of platelet-derived adhesion molecules and MPV (11-15). Platelet activation markers are elevated regardless of HF pathogenesis (14,16), with the severity of AHF correlated with the degree of platelet activation (17,18).
Table 1. Demographic and laboratory parameters in patients with and without AHF.
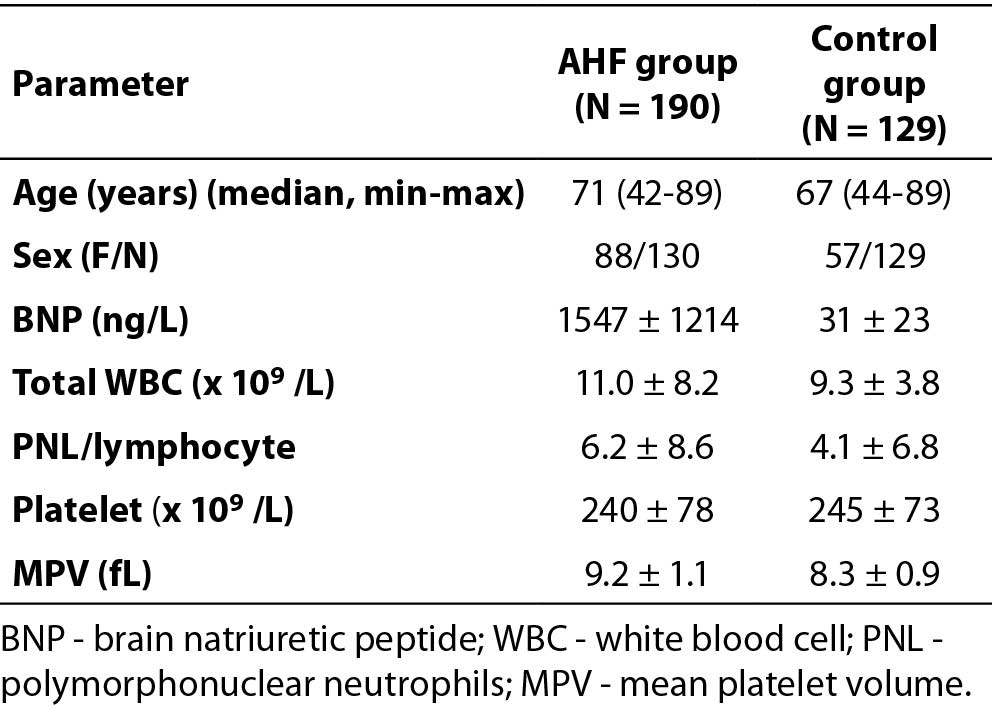
Table 2. Correlation of BNP with biochemical parameters in all patients (N = 319).
Activation of platelets can be evaluated by various techniques, including optical aggregometry, platelet function analysis using a PFA-100 system, platelet reactivity tests, platelet aggregate ratio measurements, flow cytometry and thromboxane B2 generation tests (19). The specificity and reproducibility of these assays are poor, limiting their clinical use (19). In contrast, MPV is a simple marker that does not require advanced or expensive technology.
The activation of neurohormonal, inflammatory, and thrombotic pathways (20-22) has been found to be associated with enhanced platelet reactivity in patients with AHF (14,23-26). MPV has emerged as a relatively reliable marker of inflammation in patients with various diseases (27,28), with high MPV associated with low-grade inflammation. BNP concentration was positively correlated with MPV and PNL/L ratio, which indicates a direct role of platelet activation in the pathophysiology of AHF.
We also found that BNP concentration was positively correlated with PNL/L ratio. Leukocyte count has been reported to be a predictor of heart failure (29), as well as with the development of heart failure and one-year mortality rates in patients with MI (30). In patients with chronic HF, however, a low lymphocyte count or low percentage of lymphocytes has been associated with patient mortality (31,32).
This study had several limitations. One limitation was the use of EDTA as an anticoagulant, since EDTA increases nominal platelet volume. However, EDTA was found to increase MPV by only 3.4% after 60–120 minutes (33). Moreover, most studies using EDTA have avoided the period of rapid change by waiting 1–4 hours after collection before measuring MPV (33). Because our patients were seen in the emergency room, their blood cell counts were measured within 30 minutes after blood was taken.
The design of the present study is cross-sectional and thus cannot confirm a causal relationship. BNP concentration was assessed at a single point in time, and MPV is a nonspecific marker of platelet activation which can occur under various conditions. Moreover, the relatively small sample size affected the power of this study. Some of these patients were under antiplatelet therapy for their conditions which might affect our results. However, there are reports that found no significant association between increased MPV and antiplatelet therapy (34,35).
Because this study was retrospective, we could not perform additional tests to determine the nature of the relationships among BNP, MPV and ventricular dysfunction in patients with HF.
Conclusion
Our findings indicate that MPV values correlate with BNP concentration, an indicator of HF severity and clinical status, in patients with AHF admitted to the emergency department. Further prospective studies are needed to clarify these findings.


